Throughout the year, Harvard Stem Cell Institute (HSCI) supporters are invited to calls hosted by Co-Directors Douglas Melton and David Scadden. There, supporters have the opportunity to make direct connections with HSCI scientists who are leaders in their field, learning about new advances and asking burning questions. Here, we share highlights from the Directors’ Calls of 2021.
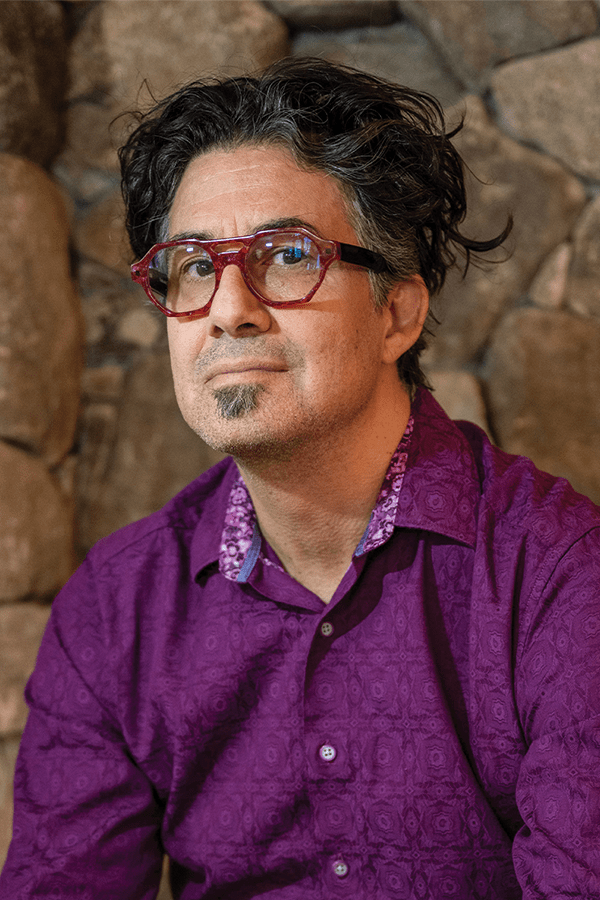
Derrick Rossi, Ph.D.
Co-Founder of Moderna Therapeutics
Former HSCI Principal Faculty member
Question: I don’t need to introduce Moderna to people nowadays: many of us have received the benefits of a Moderna COVID-19 vaccine. That is in no small part due to Derrick’s imagination about how to use messenger RNA to affect biomedicine. Derrick, I would hazard a guess that you didn’t have any idea of the impact that it would have on humanity. What was going through your head at the time?
Answer: The ability to differentiate cells back to stem cells took the world by storm. This project that we were doing was using a modified mRNA to reprogram differentiated cells back to potency.
HSCI is very good at recognizing high-risk science that has potential and funding it. As soon as we made a few dozen human proteins, it became obvious to me what we could use this for: if you could make protein so readily, you had a handle on human disease. Now that has been realized with the vaccine.
Q: You were not necessarily thinking of the applications when you were first doing your work. And yet, something allowed you to be able to move it forward.
A: I happen to be fortunate to be doing my work at Harvard Medical School and within the greater ecosystem of Boston and Cambridge, which is the absolute dead center of biotech enterprise on planet Earth. This concentration of science, business development, intellectual property, venture capital, and philanthropy was critical — the greater the concentration, the better. This might not have happened had it not been for that.
Amy Wagers, Ph.D.
Harvard University
HSCI Executive Committee member, Musculoskeletal Program Co-Leader, and Principal Faculty member
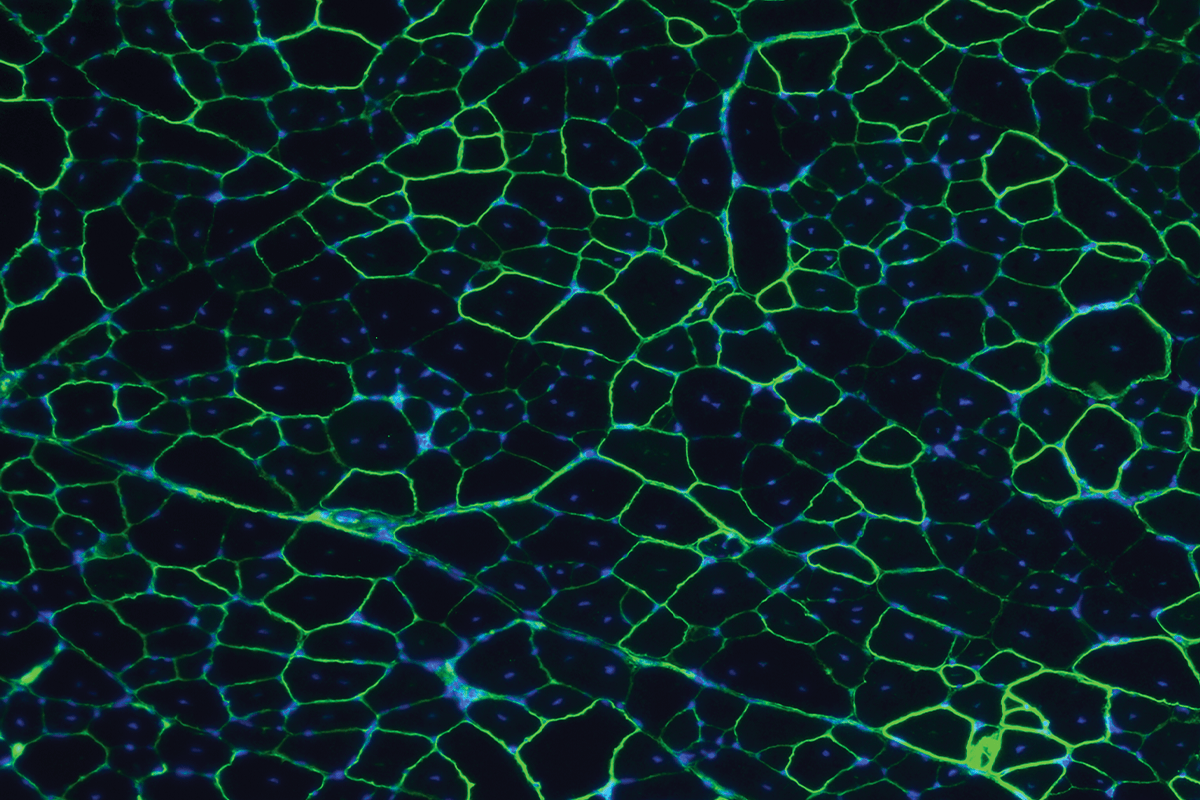
Q: Amy has done some really beautiful work on identifying ways in which we can correct muscle diseases, particularly the terrible genetic diseases of muscular dystrophy. Can you share what you’ve been able to figure out?
A: What’s really held back the field has been an inability to deliver gene therapies safely, effectively, and specifically to the relevant cell types. These approaches have largely made use of adeno-associated viral vectors, or AAVs, which can encapsulate genes and deliver them into the muscle tissue. But they also deliver to other tissues including — particularly problematically — to the liver, which can lead to toxicity.
This is where our work comes in. We made a huge library of randomly modified variants of the virus. Each virus carried a gene to detect the few virus particles among the millions that were actually able to functionally deliver their cargo into muscle. Applying this system in mice, we identified a very large class of muscle-directed AAVs that we named MyoAAVs.
Understanding the mechanism underlying the delivery profile of these vectors enabled their evolution to even more potent forms: the second-generation MyoAAVs showed up to 80-times greater delivery to skeletal muscle and showed remarkably enhanced therapeutic potency. We’ve also identified third- and fourth-generation MyoAAVs that have robust delivery to primate muscle. We can now test these vectors in models of severe genetic muscle diseases, including Duchenne muscular dystrophy.

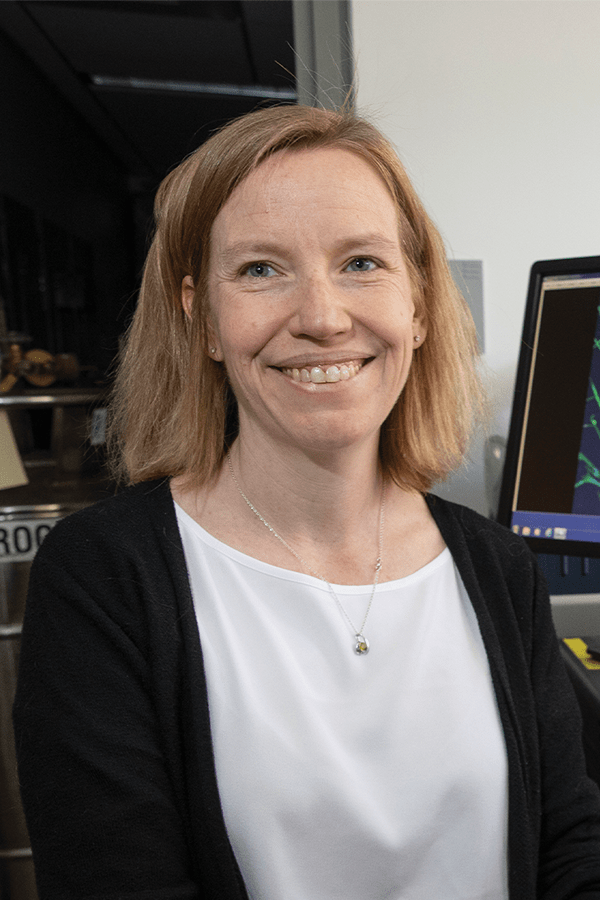
Christiane Wrann, D.V.M., Ph.D.
Massachusetts General Hospital
HSCI Affiliate Faculty member
Q: We all know that exercise is good for you, but Christiane has delved into this deeply to say what is really the molecular basis of improvements. What are the possible mechanisms that link exercise and brain function?
A: The novel exercise hormone that we’re interested in is called irisin. This is a molecule that is expressed in skeletal muscle and in the hippocampus, the part of the brain that’s important for learning and memory, and also one of the brain regions that first declines in aging and Alzheimer’s disease. We have shown that irisin carries the cognitive benefits of exercise.
If you have a very small molecule such as irisin that travels in the bloodstream to the brain, then it is feasible to turn it into a drug. In several mouse models of Alzheimer’s disease, we saw a significant improvement in cognitive function of the mice treated with irisin.
Q: It looks like irisin is on the way to being tested in a clinical trial. How do you imagine bringing this forward to patients?
A: We recognize that Alzheimer’s disease is very difficult to tackle, however we are optimistic this has some chances. It’s possible that Parkinson’s is one of the other diseases where irisin has an effect. We feel this is an innovative, different approach which could catalyze the field.