At the Harvard Stem Cell Institute (HSCI), our researchers are finding new ways to fine-tune cell behavior. For instance, scientists can engineer therapeutic cells and direct them to eliminate disease cells. On the flip side, researchers can also target and stop the activity of abnormal cells. Together, these approaches are an important avenue for developing better treatments.
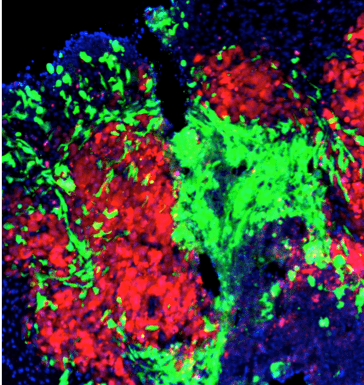
Engineering stem cells to target metastatic breast cancer
HSCI Principal Faculty member Khalid Shah, M.S., Ph.D., created engineered stem cells, directing them to eliminate breast cancer that had metastasized to the brain. The researchers analyzed patient samples, identifying two types of receptors that were important for tumor growth. The researchers then engineered stem cells with a molecule that targeted both receptor types.
In three different mouse models of brain metastasis, the engineered stem cells successfully crossed the blood-brain barrier and improved survival rates. This stem cell therapy is a promising approach for treating cancer across the blood-brain barrier, which is challenging using most therapeutics.
Image: In the mouse brain, engineered stem cells (green) target metastasized tumor cells (red). Credit: Shah Lab, Brigham and Women’s Hospital
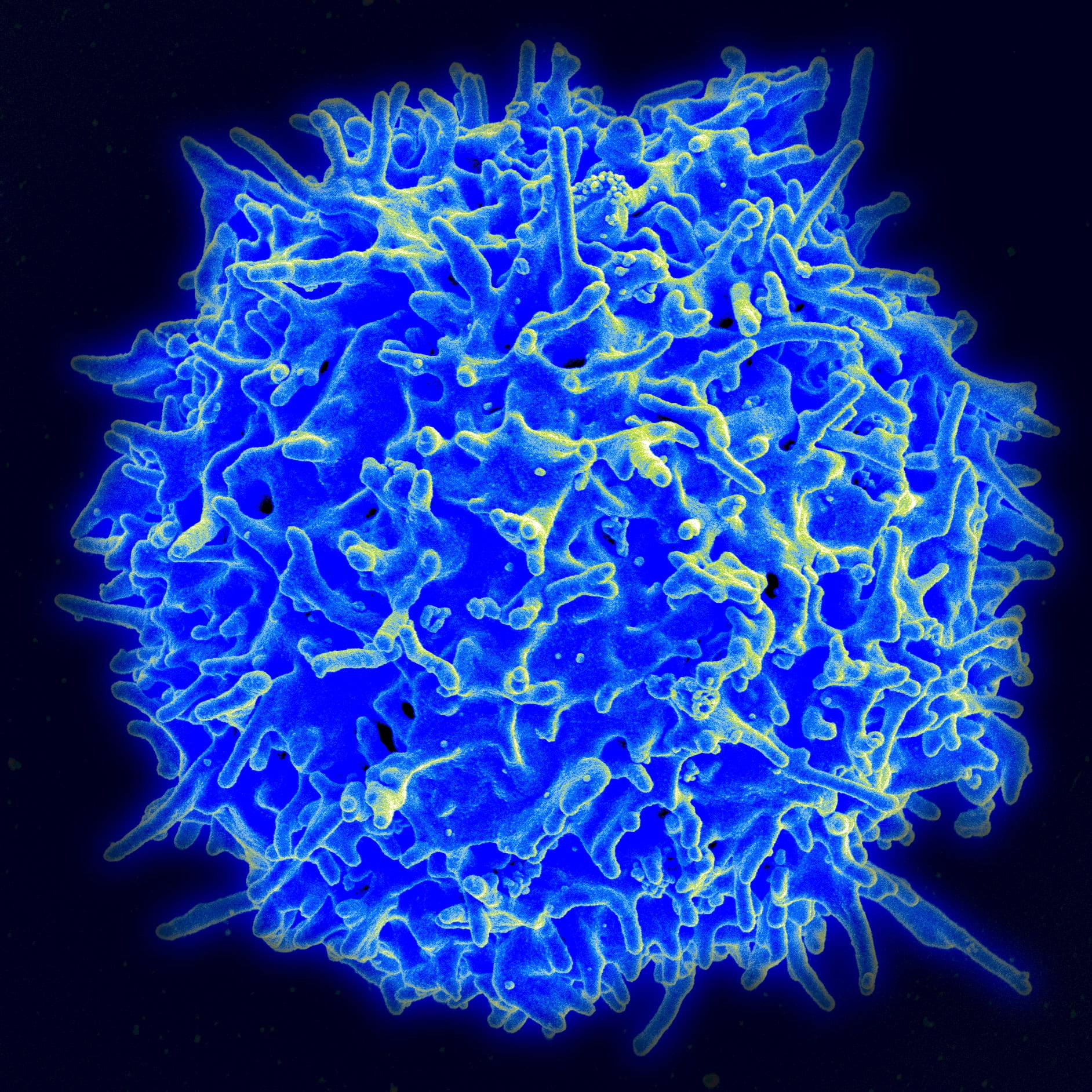
Controlling CAR T cell behavior during immunotherapy
In CAR T cell therapy, immune cells are engineered to recognize and attack harmful cells. This approach has shown success in treating certain types of advanced cancers, but CAR T cells can also trigger inflammation as a toxic side effect. HSCI researchers led by HSCI Principal Faculty member Benjamin Ebert, M.D., Ph.D., developed a way to better control the activity of CAR T cells: they engineered switchable CAR T cells that could be turned on or off by giving a commonly used cancer drug, lenalidomide.
The CAR T cells designed with a molecular “off-switch” could be quickly and reversibly turned off by administering the drug. Alternatively, CAR T cells designed with an “on-switch” only killed tumor cells during drug treatment. These approaches of improving control over CAR T cells can lead to safer and more targeted cell therapies.
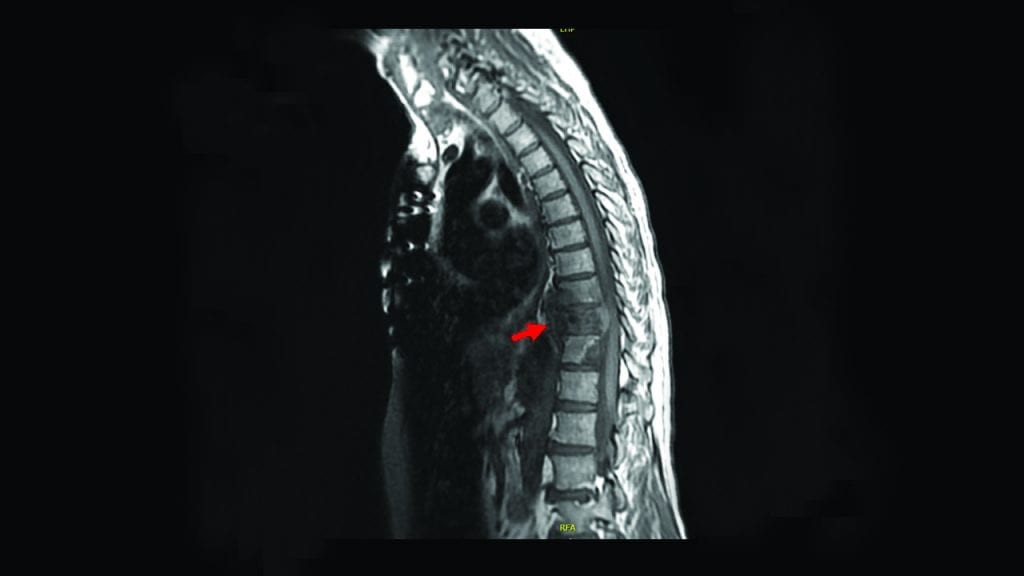
Why therapy resistance occurs in metastatic prostate cancer
HSCI researchers investigated why metastatic prostate cancer responds poorly to immunotherapy, which usually boosts the body’s own immune system to target cancer cells. The scientists were led by Affiliate Faculty member Peter Kharchenko, Ph.D., Principal Faculty member David Sykes, M.D., Ph.D., and Co- Director David Scadden, M.D.
The researchers used patient samples of prostate cancer that had metastasized to the bone marrow, asking why the cancer had evaded the immune system. They found that inside the bone marrow, the tumor caused the development of abnormal immune cells that suppressed the normal immune defenses. Blocking the suppressive signal could restore proper immune behavior and improve the animals’ survival.
Controlling the suppressive signal is a promising approach to treat metastatic prostate cancer, especially since one option is to repurpose compounds that have already been tested in people for other diseases.
Image: MRI scan of a patient’s spine, showing prostate cancer that has metastasized to the bone marrow. Credit: Philip Saylor, Massachusetts General Hospital
We found that a group of cells sends a signal that turns off the immune attack of T cells. Interrupting that signal releases the brake and the immune system can go after tumor cells enough to extend the lifespan of animals. There are agents that have been tested in humans in other settings which target the ‘off’ signal. This work supports testing them in metastatic prostate cancer.
David Scadden, M.D.